In India, primary healthcare remains inadequate, fragmented, and subpar in quality, leading to high out-of-pocket health expenditures. Current primary healthcare services in India focus heavily on Reproductive, Maternal, and Child Health and Adolescent Health (RMNCH+A) programs, neglecting the epidemiological and demographic transitions that have occurred in the country.
Currently, cardiovascular diseases, respiratory diseases, and cancers are the top three causes of mortality among young and middle-aged adults in India. India is rapidly becoming urbanized, and multiple challenges that stem out from rapid urbanization such as large-scale migration poses difficulty in the provision of comprehensive primary health care. Hence, there is a need to strengthen the urban primary health care systems to deliver comprehensive primary health care across the care continuum.
Our Approach
We have adopted an implementation research approach to design and implement a comprehensive primary health care model. As a part of this approach, we assess the primary health care situation in a particular geography, identify the gaps, design and implement local context-specific intervention packages, evaluate feasibility and effectiveness of interventions and scale-up in partnership with the local state and district governments. A dedicated formative research with concurrent monitoring approach throughout the implementation of these interventions inform us to refine interventions based on quality evidence.
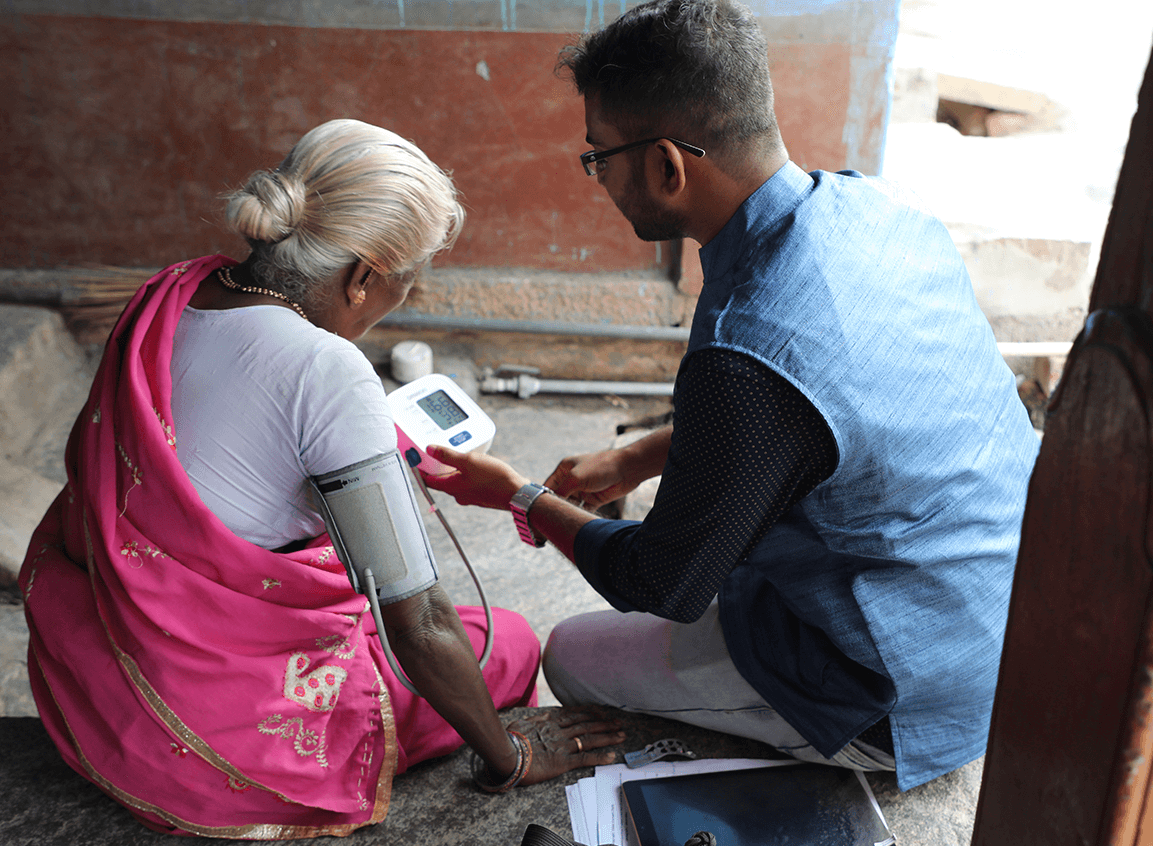
We are currently implementing a model aimed at strengthening the continuum of care for diabetes and hypertension in an urban setting. We are exploring the role of technology to improve efficiency, quality of health services and promote equitable health services by facilitating access and coverage of services across the continuum of care.
We have adopted a patient-centric approach across the NCD care continuum to bring more patient-centricity in the community outreach, mobilization, communication efforts in addition to improving quality care at the facilities to achieve better treatment outcomes Our current interventions are centered in Mysore City, Karnataka.
Our Achievements
- We provided technical support to the National Urban Health Mission (NUHM), Government of Karnataka, in conducting the training of trainers (ToT) program on implementing national NCD Program interventions.
- The Indian Council of Medical Research (ICMR) has adopted the implementation research approach, processes and tools from the Mysore project for the National Task Force Project on NCDs among tribal populations across six states in the country.
- KHPT was awarded ASSOCHAM’s “Diabetes Awareness, Prevention & Wellness Award, 2019” on World Diabetes Day.
- We presented on the topic of ‘Harnessing Technology to Improve Non-Communicable Disease Continuum of Care in Mysore City, South India’ at the 6th Global Symposium on Health Systems, 2020
Publications
- Jayanna, K., Swaroop, N., Kar, A., Ramanaik, S., Pati, M. K., Pujar, A., … Mohan, H. L. (2019). Designing a comprehensive Non-Communicable Diseases (NCD) programme for hypertension and diabetes at primary health care level: Evidence and experience from urban Karnataka, South India. BMC Public Health, 19(1), 1–12. https://doi.org/10.1186/s12889-019-6735-zb
- Pati MK, Jayanna K, Swaroop N, Arin K, Madegowda H, Mohan HL, Damme WV. Gaps in provision of integrated Primary Health Care for Non-Communicable Diseases in India. BMC Public Health Reviews, 2019.